

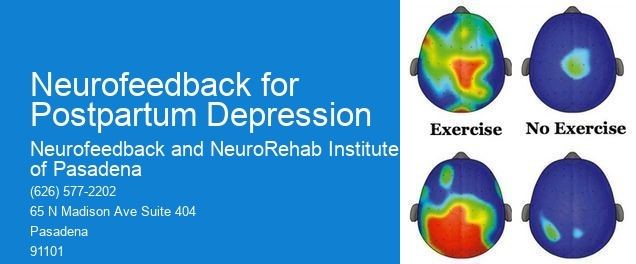
Neurofeedback therapy targets the symptoms of postpartum depression by training the brain to regulate its own activity. By providing real-time feedback on brainwave patterns, neurofeedback therapy helps individuals learn to self-regulate their brain function, leading to improved mood, reduced anxiety, and enhanced emotional stability. This can be particularly beneficial for postpartum depression as it addresses the underlying neurological imbalances that contribute to the condition, offering a non-invasive and drug-free approach to symptom management.
Alpha-Theta TrainingIn postpartum depression patients, neurofeedback therapy aims to regulate specific brainwave patterns such as alpha, beta, theta, and delta waves. Neurofeedback Practitioner By targeting these patterns, neurofeedback seeks to optimize brain function, improve emotional regulation, and reduce symptoms of depression. For example, increasing beta waves associated with alertness and focus while decreasing theta waves linked to stress and anxiety can help alleviate the symptoms of postpartum depression and promote a more balanced emotional state.
The potential benefits of using neurofeedback as a treatment for postpartum depression compared to traditional therapies include its non-invasive nature, lack of medication-related side effects, and its focus on addressing the underlying neurological imbalances. Training Protocols Neurofeedback therapy also offers a personalized approach, as it targets specific brainwave patterns unique to each individual, potentially leading to more tailored and effective treatment outcomes.
Neurofeedback therapy can be used as a standalone treatment for postpartum depression, but it is often utilized in conjunction with other therapies for comprehensive care. Combining neurofeedback with counseling, support groups, and lifestyle modifications can provide a holistic approach to addressing postpartum depression, addressing both the neurological and psychological aspects of the condition.
When considering neurofeedback therapy for postpartum depression, it's important to be aware of potential contraindications and risks, especially for breastfeeding mothers. Biofeedback Research While neurofeedback is generally considered safe, individual factors such as medication use, seizure disorders, or certain medical conditions may warrant caution. Consulting with a healthcare provider experienced in neurofeedback therapy can help assess the suitability and safety of the treatment for each individual's specific circumstances.

The timeline for noticeable improvements in postpartum depression symptoms with neurofeedback therapy can vary depending on individual factors such as the severity of symptoms, the frequency of sessions, and the individual's responsiveness to the treatment. Some individuals may experience improvements within a few weeks, while others may require several months of consistent neurofeedback sessions to achieve significant relief from symptoms.
BiofeedbackPractitioners providing neurofeedback therapy for postpartum depression should have specific qualifications and certifications in neurofeedback training and practice. Look for practitioners who are licensed healthcare professionals with additional training in neurofeedback therapy, ensuring that they have the expertise and knowledge to deliver safe and effective treatment for postpartum depression.
Neurofeedback has shown promise in addressing complex trauma disorders with comorbid conditions by targeting specific neural pathways associated with trauma responses, such as hyperarousal, dissociation, and emotional dysregulation. By utilizing real-time monitoring of brain activity and providing feedback to the individual, neurofeedback can help regulate the autonomic nervous system, enhance emotional regulation, and improve cognitive functioning. Additionally, neurofeedback can address comorbid conditions such as anxiety, depression, and attention-deficit/hyperactivity disorder by promoting neuroplasticity and optimizing brain functioning. This approach offers a personalized and non-invasive intervention that complements traditional therapeutic modalities, providing a holistic approach to addressing complex trauma disorders and their associated comorbidities.
Neurofeedback has shown promising results in addiction treatment, with studies indicating that it can be effective in reducing cravings, improving emotional regulation, and enhancing overall well-being. Research has suggested that neurofeedback may help individuals with addiction by targeting specific brain regions associated with reward processing, impulse control, and decision-making. By training the brain to self-regulate and function more efficiently, neurofeedback has the potential to support long-term recovery from addiction. While individual success rates may vary, many individuals have reported positive outcomes from incorporating neurofeedback into their addiction treatment plans. Further research and clinical trials are ongoing to better understand the specific mechanisms and efficacy of neurofeedback in addiction treatment.
Neurofeedback therapy has shown promise in benefiting both patients and caregivers in Alzheimer's disease cases. By utilizing neurofeedback techniques, individuals with Alzheimer's may experience improvements in cognitive function, memory retention, and overall quality of life. This can lead to a reduction in caregiver burden and an enhanced sense of well-being for both the patient and their caregivers. The use of neurofeedback may also contribute to a more positive caregiving experience by potentially reducing stress, anxiety, and depression among caregivers. Additionally, the potential for improved communication and interaction between the patient and caregiver may further enhance the overall care dynamic. Overall, neurofeedback therapy holds potential benefits for both patients and caregivers in the context of Alzheimer's disease.
Yes, there are neurofeedback programs specifically designed to help manage bipolar disorder in children. Neurofeedback, also known as EEG biofeedback, is a non-invasive treatment that aims to regulate brain activity and improve self-regulation. These programs often involve monitoring brainwave patterns and providing feedback to help children learn to self-regulate their emotions and behavior. Neurofeedback for bipolar disorder in children may focus on enhancing mood stability, reducing impulsivity, and improving attention and focus. It can be a valuable adjunct to traditional treatments such as medication and therapy, offering a more holistic approach to managing the symptoms of bipolar disorder in children.
The recommended duration of neurofeedback treatment for PTSD can vary depending on the individual's specific needs and response to the therapy. Typically, a course of neurofeedback treatment for PTSD may involve regular sessions over a period of several months to a year. The frequency and duration of sessions may be tailored to the severity of the PTSD symptoms, the individual's progress, and their overall treatment plan. It's important for the neurofeedback therapist to continually assess and adjust the treatment protocol based on the client's ongoing response and needs. Additionally, integrating complementary therapies and support services alongside neurofeedback may further enhance the overall treatment outcomes for individuals with PTSD.
Neurofeedback has shown promise in supporting individuals with Alzheimer's disease in maintaining cognitive function. By utilizing advanced brainwave monitoring and training techniques, neurofeedback can target specific neural pathways associated with memory, attention, and executive function, which are often affected by Alzheimer's disease. This non-invasive approach aims to modulate brain activity, enhance neural plasticity, and promote neurogenesis, potentially mitigating cognitive decline. Furthermore, neurofeedback interventions can be tailored to address individual cognitive deficits, offering personalized and targeted support for those with Alzheimer's disease. Research suggests that neurofeedback may contribute to improved cognitive performance, memory retention, and overall quality of life for individuals living with Alzheimer's disease. While further studies are needed to fully understand the long-term effects, neurofeedback presents a promising avenue for enhancing cognitive function in this population.